In recent years, the healthcare industry has witnessed a transformative shift with the integration of artificial intelligence (AI) into various facets of patient care. One notable area of impact is clinical triage—the process of determining the priority of patients’ treatments based on the severity of their condition. This article delves into the cost-effectiveness of AI-driven clinical triage systems, exploring their benefits, challenges, and the economic implications for healthcare providers.
Introduction to AI in Healthcare
Artificial intelligence, a branch of computer science focused on creating systems capable of performing tasks that typically require human intelligence, has found numerous applications in healthcare. From diagnostic imaging to personalised treatment plans, AI’s ability to analyse vast datasets and identify patterns has revolutionised patient care. The evolution of AI in medicine has been marked by significant milestones, including the development of machine learning algorithms that can predict patient outcomes and natural language processing tools that assist in clinical documentation.
Understanding Clinical Triage
Clinical triage is a critical component of emergency medicine and routine healthcare delivery. It involves assessing patients’ conditions to prioritise care, ensuring that those with the most urgent needs receive immediate attention. Traditional triage methods rely heavily on the clinical judgment of healthcare professionals, supported by established protocols and guidelines. While effective, these methods can be subjective and may vary between practitioners.
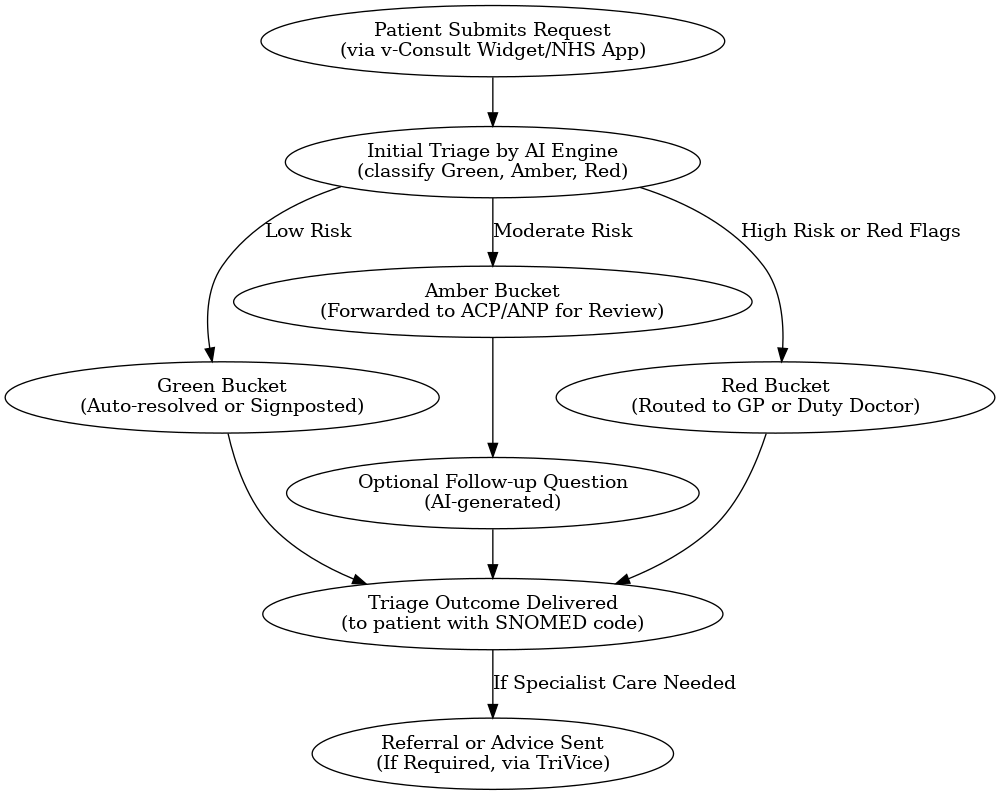
Integration of AI in Clinical Triage
The integration of AI into clinical triage processes aims to enhance decision-making by providing data-driven insights. AI-driven triage systems analyse patient data, including symptoms, medical history, and vital signs, to predict the severity of conditions and recommend appropriate care pathways. For instance, AI algorithms can evaluate electronic health records (EHRs) to identify high-risk patients who may require expedited treatment.
Benefits of AI-Driven Triage
One of the primary advantages of AI-driven triage is improved accuracy in patient assessment. By leveraging large datasets, AI systems can identify subtle indicators of severe conditions that may be overlooked during manual evaluations. Additionally, these systems can reduce waiting times by streamlining the triage process, allowing healthcare providers to allocate resources more efficiently.
Cost Implications of Traditional Triage
Traditional triage methods, while effective, can be resource-intensive. The reliance on human assessment necessitates significant staffing, and variability in evaluations can lead to inefficiencies, such as unnecessary admissions or delayed treatments. These factors contribute to increased operational costs and can strain healthcare budgets.
Economic Advantages of AI Implementation
Implementing AI-driven triage systems offers several economic benefits. Operational costs can be reduced through decreased reliance on human resources and improved patient flow management. For example, a study demonstrated that AI-enhanced heart failure screening was cost-effective, with a cost-effectiveness ratio of $27,858 per quality-adjusted life year.
Challenges in Implementing AI Triage Systems
Despite the potential benefits, several challenges exist in implementing AI-driven triage systems. The initial investment for technology acquisition and ongoing maintenance can be substantial. Additionally, healthcare professionals require training to effectively utilise these systems, and there may be resistance to adopting new technologies due to concerns about reliability and workflow integration.
Return on Investment (ROI) Analysis
Evaluating the return on investment for AI-driven triage systems involves assessing both direct and indirect financial benefits. Metrics such as reduction in patient wait times, decreased hospital admissions, and improved patient outcomes contribute to the overall ROI. Over time, the financial gains from increased efficiency and enhanced care quality can offset the initial implementation costs.
Impact on Patient Outcomes
AI-driven triage systems have the potential to significantly improve patient outcomes. By providing timely and accurate assessments, these systems facilitate early interventions, which can prevent condition deterioration and reduce the likelihood of complications. Enhanced patient satisfaction is also a notable benefit, as individuals experience more streamlined and responsive care.
Comparative Studies: AI vs. Traditional Triage
Comparative studies have highlighted the advantages of AI-driven triage over traditional methods. For instance, research indicates that AI-based triage strategies can lower projected costs by 37% compared to traditional approaches, while also averting additional disability-adjusted life years.
Ethical and Legal Considerations
The deployment of AI in clinical settings raises important ethical and legal considerations. Ensuring data privacy and maintaining patient confidentiality are paramount, necessitating robust security measures. Additionally, adherence to regulatory standards and obtaining appropriate certifications are critical to ensure compliance and build trust among stakeholders.
Future Trends in AI Triage
The future of AI-driven triage is poised for further advancements, with emerging technologies enhancing system capabilities. Developments in machine learning algorithms, integration with wearable health devices, and real-time data analytics are expected to further improve the accuracy and efficiency of triage systems. These innovations hold the promise of more personalised and proactive patient care.
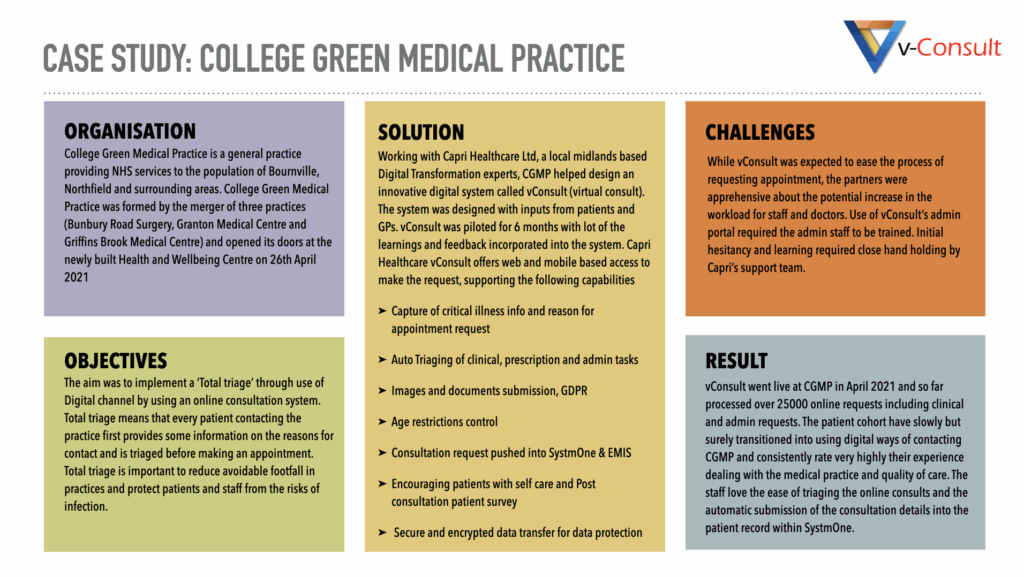
Case Study: Successful AI Triage Implementation
A notable example of successful AI triage implementation is the use of AI-powered software in hospitals to prioritise high-risk patients on waiting lists. The system, trained on over 200 million records, assesses various risk factors to identify patients who may deteriorate while waiting for treatment. This approach has led to significant improvements in patient outcomes and operational efficiency.