Introduction: The Importance of Clinical Safety
In healthcare, clinical safety is paramount. Digital health solutions must prioritise patient well-being while enhancing efficiency. TriVice, a digital triage and referral management system, incorporates clinical safety principles to support effective healthcare decision-making. This article explores the significance of clinical safety in digital solutions and how systems like TriVice align with NHS standards.
Understanding Clinical Safety in Digital Health
Defining Clinical Safety
Clinical safety involves the identification, assessment, and mitigation of risks associated with health IT systems. Errors in digital healthcare, such as incorrect referrals or data misinterpretation, can have serious consequences. A structured approach to safety ensures patient trust and system reliability.
Key Aspects of Clinical Safety in Digital Systems
A well-structured Clinical Risk Management System should adhere to established guidelines such as DCB0129 and DCB0160. Key elements include:
- Hazard identification: Recognising risks in clinical workflows.
- Risk assessment: Evaluating potential patient safety concerns.
- Risk mitigation: Implementing strategies to reduce risks.
- Ongoing monitoring: Updating safety measures based on new data and feedback.
Clinical Risk Management in Digital Health Systems
Identifying and Assessing Risks
Health IT systems must identify potential hazards and assess their impact on patient care. Common risks include misidentification, data accuracy concerns, and referral delays. These risks must be continuously reviewed and addressed.
Compliance with NHS Clinical Safety Standards
To ensure safety and compliance, digital health solutions must align with NHS Digital Clinical Safety Assurance Framework guidelines:
- Systematic assessment of clinical risks before deployment.
- Engagement with clinicians and governance teams in safety reviews.
- Regular updates to align with evolving healthcare safety standards.
Additionally, as per the Review of Digital Clinical Safety Standards DCB0129 and DCB0160, NHS Digital highlights the importance of:
- Clarifying safety obligations for both suppliers and healthcare organisations.
- Enhancing interoperability and system integration safety.
- Incorporating artificial intelligence considerations in clinical risk assessment.
- Strengthening incident reporting mechanisms to improve patient safety outcomes.
DCB0129 and DCB0160: The Pillars of Clinical Safety
DCB0129, titled “Clinical Risk Management: Its Application in the Manufacture of Health IT Systems”, provides essential guidelines for health IT system developers. It ensures that manufacturers implement clinical risk management processes throughout the system lifecycle, reducing potential risks to patients and clinicians.
On the other hand, DCB0160, “Clinical Risk Management: Its Application in the Deployment and Use of Health IT Systems”, focuses on organisations implementing digital health solutions. It requires healthcare providers to assess and manage clinical risks associated with new technologies, ensuring safe use and minimising unintended harm.
By following these two standards, digital health systems like TriVice align with NHS best practices, ensuring patient safety at both the development and deployment stages.
Features Supporting Clinical Safety in Digital Health Systems
Structured Risk Mitigation
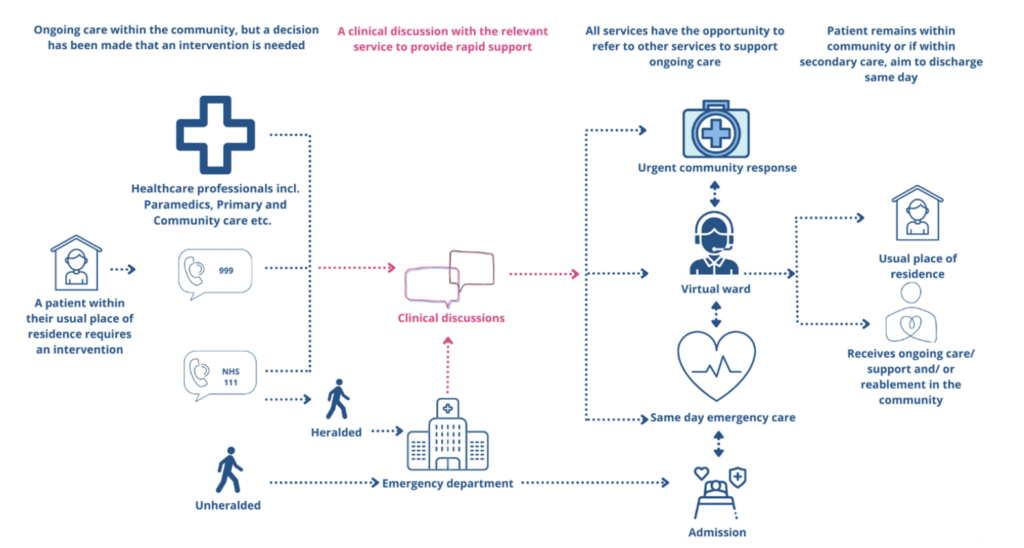
Clinical safety is enhanced when systems incorporate evidence-based risk mitigation strategies. Digital platforms should integrate risk assessment tools and structured pathways to support clinical decision-making.
Secure Data Handling
Patient data must be protected through compliance with data security standards such as ISO27001. Encryption protocols, audit trails, and access control are essential to maintaining data integrity.
Continuous Feedback for System Improvement
Establishing a real-time feedback mechanism between users and developers helps refine clinical safety measures. Regular reviews by clinicians ensure that digital tools remain aligned with best practices.
The Future of Clinical Safety in Digital Health
As healthcare increasingly relies on digital solutions, maintaining robust clinical safety frameworks will be critical. Future advancements may include greater integration of AI for risk prediction, improved interoperability between systems, and enhanced real-time monitoring tools. The NHS’s updated approach to DCB0129 and DCB0160 reinforces the need for ongoing regulatory alignment as technology evolves.
Advancing Clinical Safety in Digital Healthcare
Ensuring clinical safety in digital health requires a proactive approach to risk assessment and compliance. By aligning with regulatory standards and continuously refining safety protocols, digital healthcare systems can support better patient outcomes and improved clinical workflows.