Introduction
Head and neck cancer referrals require swift diagnosis and treatment to improve survival rates. However, inefficiencies in the referral process often lead to delays. The integration of AI-driven triage systems, such as TriVice, offers a solution by automating referrals and prioritising urgent cases.
This article explores the challenges, the current NHS referral pathway, and how AI is transforming head and neck cancer referrals.
Understanding Head & Neck Cancer Referrals
Head & Neck Cancer Referrals are critical for early detection and effective treatment. These referrals originate when a general practitioner (GP) suspects cancer and sends the patient to a specialist.
Common Symptoms Leading to Referrals
- Persistent sore throat or hoarseness
- Lumps in the neck
- Difficulty swallowing
- Unexplained weight loss
- Non-healing mouth ulcers
Importance of Timely Referrals
Delays in referrals can lead to disease progression, making treatment more complex and less effective. Early intervention improves survival rates by up to 70% in some head and neck cancer cases.
Challenges in Head & Neck Cancer Referrals
Despite established referral pathways, several challenges hinder timely diagnosis.
1. High Volume of Referrals
The NHS processes a large number of head & neck cancer referrals monthly. Many of these cases do not result in a cancer diagnosis, leading to unnecessary specialist consultations and wasted resources. Less than 10% of head & neck cancer referrals actually result in a cancer diagnosis.
2. Delayed Diagnostics
- Waiting times for CT scans, MRIs, and biopsies remain a significant issue.
- Limited specialist availability increases delays in consultations.
- Infrastructure constraints in underfunded areas lead to bottlenecks.
According to NHS England, 62-day cancer treatment targets are regularly missed, with only 70% of patients starting treatment within the required timeframe.
3. Incomplete Referral Information
Many referrals lack critical details, requiring follow-ups and delaying specialist reviews. Around 15-20% of cancer referrals need additional GP follow-up due to missing information.
4. Communication Gaps
Lack of real-time updates between GPs, specialists, and diagnostic centers results in:
- Duplicate referrals
- Missed follow-ups
- Patient uncertainty
A study found that 40% of GPs do not receive timely updates on their patients’ referral status.
5. Meeting Faster Diagnostic Standards (FDS)
The NHS aims to diagnose 80% of cancer cases within 28 days by 2026, but current estimates show only 77% of cases meet this target.
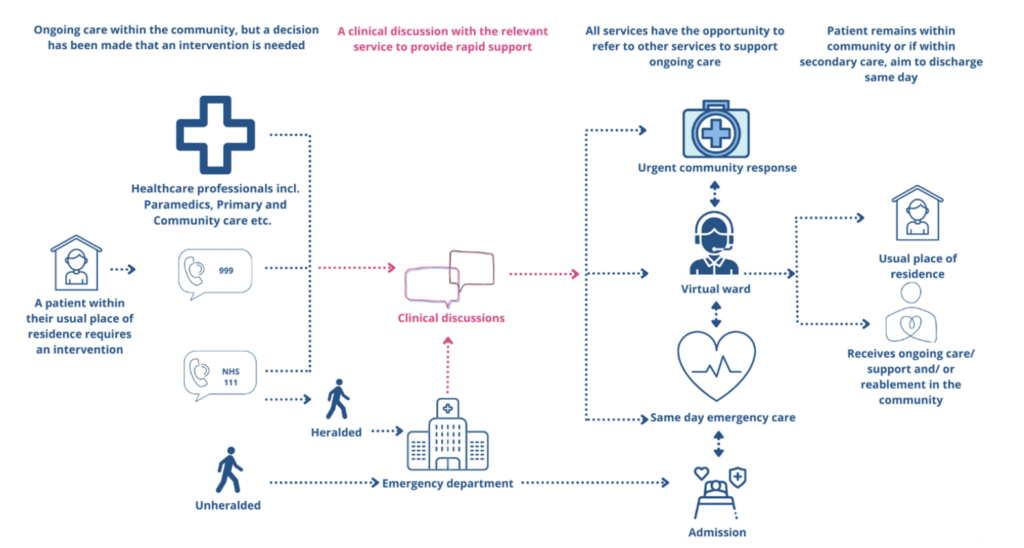
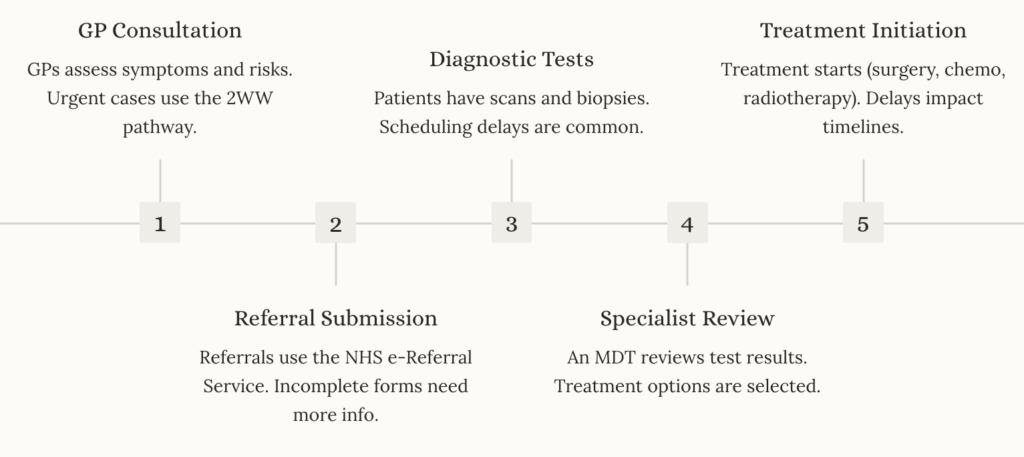
Current NHS Cancer Referral Pathway
How AI is Transforming Head & Neck Cancer Referrals
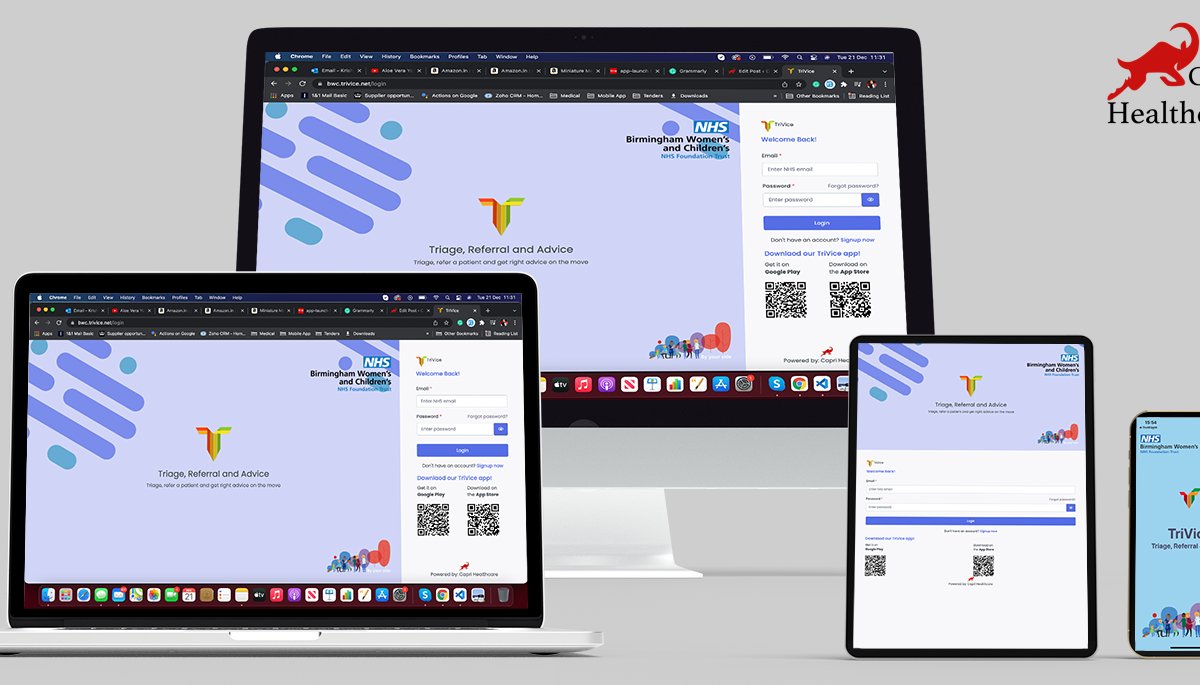
AI-driven triage systems like TriVice are revolutionising referral management by reducing inefficiencies.
1. Automated Referral Triage
TriVice uses AI algorithms to:
- Prioritise urgent cases
- Reduce unnecessary specialist appointments
- Ensure referrals contain complete details
2. Real-Time Assessment
AI evaluates patient data instantly, allowing specialists to focus on high-priority cases.
3. Decision Support for GPs
- GPs receive AI-powered guidance on referral urgency.
- Helps reduce over-referrals and improves diagnostic accuracy.
4. Faster Access to Diagnostics
- AI directs referrals to the most appropriate diagnostic tests.
- Reduces wait times for urgent cases.
5. Seamless Integration with NHS Systems
- Works within existing NHS digital infrastructure.
- Ensures smooth data exchange between providers.
TriVice has been shown to reduce unnecessary referrals by 30-40% and save 50 hours per month per specialty in triaging.
Key Benefits of AI in Cancer Referral Management
Specialists
- Time savings: Reduces manual triage efforts.
- Improved workload management: Prioritises high-risk cases.
- Faster access to diagnostic tests: Helps specialists make quicker decisions.
Patients
- Shorter wait times for specialist appointments.
- Faster diagnosis leads to early treatment.
- Better care coordination minimises disruptions.
The NHS
- Cost savings: Reduces unnecessary consultations.
- Enhanced efficiency: Streamlines workflows.
- Improved compliance with Faster Diagnostic Standards.
The Future of Head & Neck Cancer Referrals
1. AI-Powered Standardisation
Adopting AI solutions like TriVice across the NHS can help standardise referrals, ensuring timely care for all patients.
2. Expansion of AI Capabilities
Future developments may include:
- Predictive analytics for cancer risk assessment.
- Automated patient follow-ups to prevent delays.
3. Increased Adoption of Digital Pathways
The NHS is moving towards paperless referrals, making AI-driven platforms essential for smooth operations.
Frequently Asked Questions (FAQs)
1. How does AI improve Head & Neck Cancer Referrals?
AI automates referral triage, prioritises urgent cases, and reduces unnecessary specialist visits, ensuring faster diagnosis.
2. What are the main challenges in the current referral system?
Long wait times, high referral volume, incomplete information, and communication gaps between GPs and specialists.
3. What is the NHS Two-Week Wait (2WW) pathway?
The 2WW pathway ensures urgent cancer referrals are seen by a specialist within 14 days.
4. How does TriVice AI help doctors and specialists?
TriVice reduces administrative burden, improves referral accuracy, and allows specialists to focus on high-risk cases.
5. Can AI reduce unnecessary referrals?
Yes, AI decision-support tools help GPs identify cases that need specialist evaluation, reducing non-essential referrals.
6. What improvements are expected by 2026?
The NHS aims to diagnose 80% of cancer cases within 28 days and improve overall cancer performance targets.
Head & Neck Cancer Referrals are a vital step in early cancer detection, yet inefficiencies in the system lead to delays. AI-driven solutions like TriVice offer a promising way to streamline referrals, prioritise urgent cases, and improve patient outcomes.
As AI adoption grows within the NHS, the future of cancer referrals looks more efficient, reducing wait times and ensuring faster diagnoses for patients in need.
The references used in the article:
- TriVice AI-Triage Management System for Cancer Referrals – A specialised AI-driven triage system for cancer referrals, improving efficiency and reducing unnecessary referrals.
- Source: TriVice-AI-Triage-Management-System-for-Cancer-Referrals.pdf
- NHS Cancer Waiting Time Standards – Data on 62-day treatment targets and Faster Diagnosis Standards.
- Source: NHS England https://www.england.nhs.uk/cancer
- Cancer Research UK – Head & Neck Cancer Statistics – Information on survival rates and impact of early diagnosis.
- Source: Cancer Research UK https://www.cancerresearchuk.org
- NHS Digital – e-Referral Service – Overview of the NHS referral process and electronic submissions.
- Source: NHS Digital https://digital.nhs.uk/services/e-referral-service
- British Journal of General Practice – Challenges in GP Referrals – Study on incomplete referrals and communication gaps in the NHS.
- Source: BJGP https://bjgp.org